Pediatric Standers for Disabled Children
Pediatric Standers are therapeutic, adaptive equipment, or standing aides for children with physical disabilities. A stander is a frame that holds the patient in various positions, including upright, prone, and supine. It provides weight-bearing support to enable patient mobility in an upright or other position. Standing frames for children with special needs help improve their quality of life, classroom participation, and leisure activities. A s
Pediatric Standing Frames
Why Use a Stander for Disabled Children?
What are the Benefits of a Standing Frame?
What Advantages Do Standing Frames for the Disabled Offer?
What are the Types of Standers?
How to Select the Best Pediatric Stander?
Medical Studies
Why Use Special Needs Stander?
Medical studies find that some disabled patients benefit from remaining in specific positions for a specified time. One study examined 30 separate studies, concluding the following:
"Standing programs 5 days per week positively affect bone mineral density (60 to 90 min/d); hip stability (60 min/d in 30° to 60° of total bilateral hip abduction); range of motion of hip, knee, and ankle (45 to 60 min/d); and spasticity (30 to 45 min/d)."1
What are the Benefits of a Pediatric Stander?
Standers offer a host of benefits to pediatric patients, including the paraplegic. These benefits include increased circulation, reduced swelling, improved bladder function, and increased strength. They support weight-bearing and promote the use of arms and hands. A study involving school-based physical therapist found "multiple benefits with pressure relief rated very important most frequently. More than 50% of respondents indicated social and educational benefits are very important."2 The benefits of stander devices extend beyond the physical to also include social and emotional.
Stand Up Frame Advantages
- enhances circulation
- reduces swelling
- improves bone density
- supports skeletal development
- manages scoliosis
- improves bowel function
- enhances kidney function
- promotes bladder function
- strengthens trunk muscles
- strengthens leg muscles
- enhances head controls
- prevents/manages pressure ulcers
- manages atrophy
- helps to stimulate a range of motion
- strengthens cardiovascular
- encourages head control
- improves respiratory function
- stimulates gastric motility
- encourages motor development
- psychological boost to the patient by placing them at eye level with other children
- supports hip alignment
- reduces the risk of lower extremity contractures
What are the Types of Special Needs Standers?

 supine stander - provides posterior support for children that cannot support their head
supine stander - provides posterior support for children that cannot support their head prone stander - leans forward to offer anterior support for children that can support their head
prone stander - leans forward to offer anterior support for children that can support their head vertical stander - supports an upright position for children with some balance and trunk control
vertical stander - supports an upright position for children with some balance and trunk control  multi-position stander - adjustable to provide two or more types of support
multi-position stander - adjustable to provide two or more types of support sit-to-stand stander - assist patients with transfers between vertical to supine positions
sit-to-stand stander - assist patients with transfers between vertical to supine positions mobile stander - an upright self-propulsion stander that offers partial weight-bearing to enable an upright position and upper mobility. It promotes motor skills and independence by offering more patient mobility functions leading to independent standing.
mobile stander - an upright self-propulsion stander that offers partial weight-bearing to enable an upright position and upper mobility. It promotes motor skills and independence by offering more patient mobility functions leading to independent standing. motorized stander - dynamic standers offer intermittent weight bearing to improve bone density3 (These devices are not in wide use and have so far demonstrated limited usefulness.)
motorized stander - dynamic standers offer intermittent weight bearing to improve bone density3 (These devices are not in wide use and have so far demonstrated limited usefulness.)
The basic standers are vertical, prone, and supine. The advanced standers include the multi-position, sit-to-stand, and mobile standers. The advanced devices provide more adjustments to meet the changing needs of the patient. These devices are adjustable as the patient increases in capacity and skills. This adaptability helps to move patients from one skill level to another.
How to Select the Best Pediatric Stander
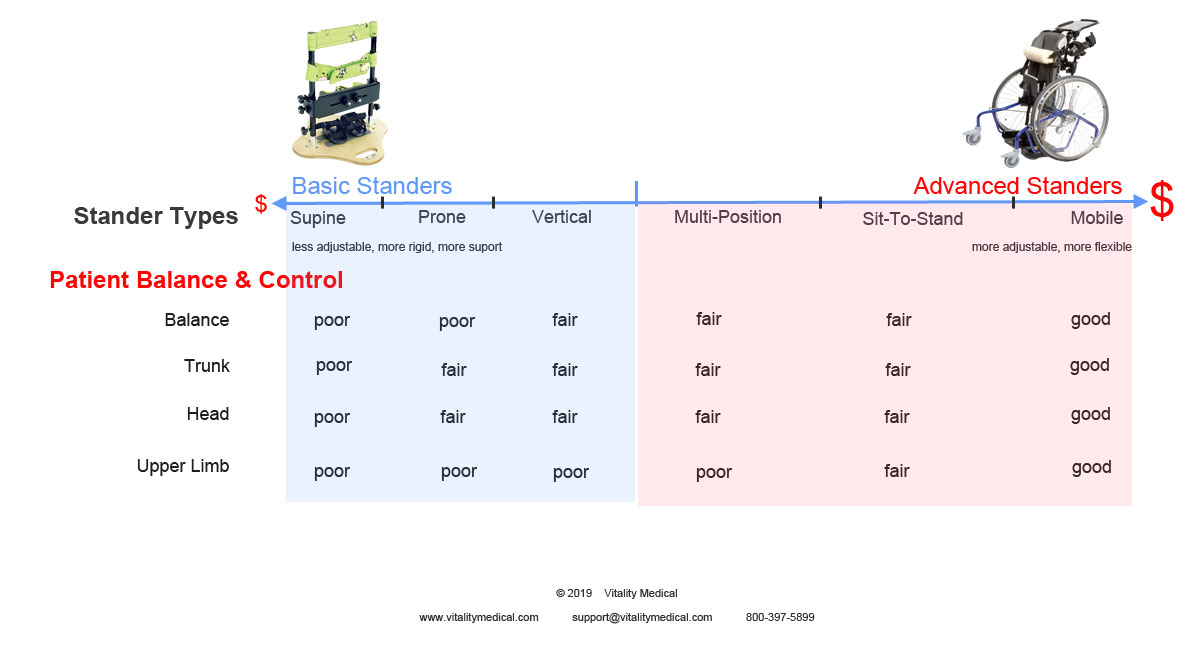
Choosing the right pediatric stander is not a daunting task. Displayed in the product continuum above are the basic standing frames on the left and the advanced on the right. Moving from left to right along the continuum, we see that the price is more likely to increase as the stand up frame becomes more adjustable, flexible, and adaptable. The patient factors of balance and control located below the continuum line match vertically with your most likely best option. The more balance and control that the patient has, the more advanced the stander to accommodate their abilities.
Footnotes
- 1. Paleg, Ginny S., Beth A. Smith, and Leslie B. Glickman. "Systematic review and evidence-based clinical recommendations for dosing of pediatric supported standing programs." Pediatric Physical Therapy 25.3 (2013): 232-247.
- 2. Taylor, Kristin. "Factors affecting prescription and implementation of standing-frame programs by school-based physical therapists for children with impaired mobility." Pediatric Physical Therapy 21.3 (2009): 282-288.
- 3. Gudjonsdottir, Bjorg, and V. Mercer Stemmons. "Effects of a dynamic versus a static prone stander on bone mineral density and behavior in four children with severe cerebral palsy." Pediatric physical therapy: the official publication of the Section on Pediatrics of the American Physical Therapy Association 14.1 (2002): 38-46.
Medical Studies
-
 Paleg, Ginny S., Beth A. Smith, and Leslie B. Glickman. "Systematic review and evidence-based clinical recommendations for dosing of pediatric supported standing programs." Pediatric Physical Therapy 25.3 (2013): 232-247.
Paleg, Ginny S., Beth A. Smith, and Leslie B. Glickman. "Systematic review and evidence-based clinical recommendations for dosing of pediatric supported standing programs." Pediatric Physical Therapy 25.3 (2013): 232-247. -
 Taylor, Kristin. "Factors affecting prescription and implementation of standing-frame programs by school-based physical therapists for children with impaired mobility." Pediatric Physical Therapy 21.3 (2009): 282-288.
Taylor, Kristin. "Factors affecting prescription and implementation of standing-frame programs by school-based physical therapists for children with impaired mobility." Pediatric Physical Therapy 21.3 (2009): 282-288. -
 Gudjonsdottir, Bjorg, and V. Mercer Stemmons. "Effects of a dynamic versus a static prone stander on bone mineral density and behavior in four children with severe cerebral palsy." Pediatric physical therapy: the official publication of the Section on Pediatrics of the American Physical Therapy Association 14.1 (2002): 38-46.
Gudjonsdottir, Bjorg, and V. Mercer Stemmons. "Effects of a dynamic versus a static prone stander on bone mineral density and behavior in four children with severe cerebral palsy." Pediatric physical therapy: the official publication of the Section on Pediatrics of the American Physical Therapy Association 14.1 (2002): 38-46. -
 Caulton, J. M., et al. "A randomised controlled trial of standing programme on bone mineral density in non-ambulant children with cerebral palsy." Archives of Disease in Childhood 89.2 (2004): 131-135.
Caulton, J. M., et al. "A randomised controlled trial of standing programme on bone mineral density in non-ambulant children with cerebral palsy." Archives of Disease in Childhood 89.2 (2004): 131-135.











Login and Registration Form